Well there you go then my point was that it's mind numbingly boring. If you want people to be more active to live a healthier life and prevent strain on the healthcare system, promote shit that people like rather than mindlessly running or picking shit up and putting it back down again.No but people that can't grasp the nature of its purpose are pretty short sighted. I agree though that finding an activity you like is very important. Doing both is best case scenario.
Options for the NHS
- Thread starter Red in STL
- Start date
-
 In the latest episode of the United Hour Podcast, Nik (@Rood) and Imran (@Annihilate Now!) are here to discuss three 1-1 draws.
In the latest episode of the United Hour Podcast, Nik (@Rood) and Imran (@Annihilate Now!) are here to discuss three 1-1 draws.
The first got us knocked out of the FA Cup, the next puts us in a good position in our Round of 16 Europa League game, and the latest was an actual decent performance against Arsenal at Old Trafford.
All hopes for the season now rest on the Europa League - does Amorim have the squad to win it?
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
It doesn't seem like you've read her (apologies for the wrong pronoun) comment.Yes I did read her comment.
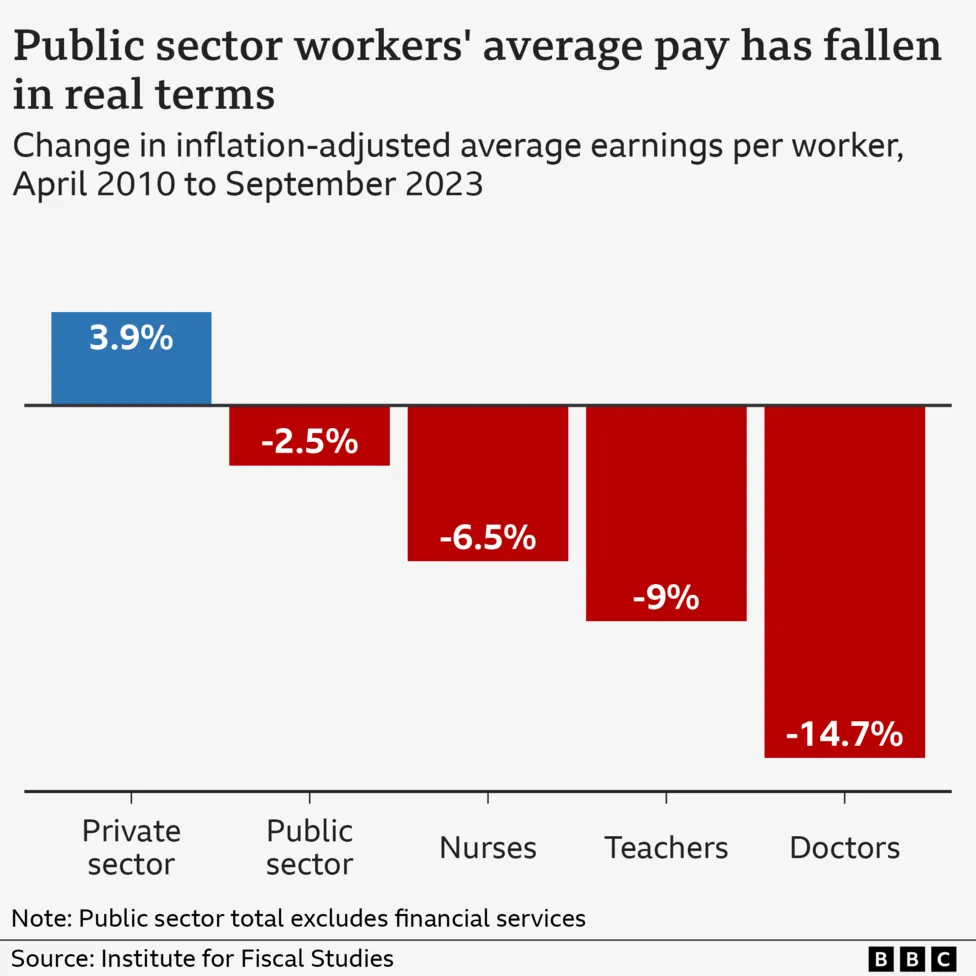
If the BMA was so successful in aggressively pushing the interests of its members, you have to wonder why discontent is so high at every level of the system, in both primary and secondary care.
Why retention is becoming so poor and why many physicians are looking jealously at the salaries and working conditions of their peers across the anglosphere, much of western and northern Europe and even increasingly back home to countries that many would consider lesser economies than the UK's?
RedC
Votes Fine Gael.
- Joined
- Feb 19, 2011
- Messages
- 7,084
Literal millions of people enjoy running and the gym.Well there you go then my point was that it's mind numbingly boring. If you want people to be more active to live a healthier life and prevent strain on the healthcare system, promote shit that people like rather than mindlessly running or picking shit up and putting it back down again.
I never said they didn'tLiteral millions of people enjoy running and the gym.

africanspur
Full Member
- Joined
- Sep 1, 2010
- Messages
- 10,012
- Supports
- Tottenham Hotspur
It doesn't seem like you've read her (apologies for the wrong pronoun) comment.
Why, which bit do you think I've not read?
The part where she's said they are not belonging to the NHS and have very favourable terms (no out of hours appointments and extra pay for various bits). She also appears to be or has been in the past, quite involved with the whole process so I'm willing to listen to what she's saying.Why, which bit do you think I've not read?
africanspur
Full Member
- Joined
- Sep 1, 2010
- Messages
- 10,012
- Supports
- Tottenham Hotspur
The part where she's said they are not belonging to the NHS and have very favourable terms (no out of hours appointments and extra pay for various bits). She also appears to be or has been in the past, quite involved with the whole process so I'm willing to listen to what she's saying.
So how did I not read it?
Nothing I said indicates that I didn't read the post. I'm saying that somehow, despite the BMA apparently being this boogeyman who gets amazing terms for GPs. Yet despite this, a third of GPs want to quit within 5 years. 20% of (fully qualified!!) GPs under the age of 30 quit last year.
Why people think doctors should be paid the same for working on a Sunday morning as a Tuesday afternoon I have no idea really. I certainly wouldn't expect to be paying a plumber or lawyer the same.
I've worked as a (hospital) doctor in 4 different countries and have friends and colleagues working in others which I have not. Through circumstance that I won't bother getting into, the UK is where I've ended up staying and working and honestly the way doctors are seen here in this country compared to the other countries is....baffling.
T00lsh3d
Has massive thighs.
- Joined
- Mar 20, 2014
- Messages
- 10,365
I went for an executive board-level job at the trust earlier this year (having worked exclusively in the private sector). As part of the interview process I did an engagement exercise with the directors of various specialties and operating departments. They were the most soulless uninspiring group of people I’ve ever sat with. Less energy and optimism than at a funeral. After an hour I knew that this was a group of people clinging to their salaries and pension, who lacked the passion and capability to change things for the better. It was eye-opening and there was no way I’d spend the rest of my life working around such misery
Red in STL
Turnover not takeover
I'm glad I started this thread, it seems quite a few posters have observations that are worthy of more discussion, for my part I'll add this:
In the US as an alternative to A&E (or the ER as they call it here) most areas have a number of what's called Urgent Care facilities, I know that the UK has some of these but just how widespread and accesible are they?
In my local area the main hospital is 3 miles away and in a 5 mile radius there's at least half a dozen of these facilities, they're open 8am to 8pm 7 days a week and are first come, first served with no appointments.
They're mostly staffed by nurse practitioners but there is always at least one doctor on-site as well, my family have used these from time-to-time over the years (getting GP appointments is someimes as bad here as the UK) an found them to be quite good.
Maybe an expansion of this type of facility is what the UK needs?
In the US as an alternative to A&E (or the ER as they call it here) most areas have a number of what's called Urgent Care facilities, I know that the UK has some of these but just how widespread and accesible are they?
In my local area the main hospital is 3 miles away and in a 5 mile radius there's at least half a dozen of these facilities, they're open 8am to 8pm 7 days a week and are first come, first served with no appointments.
They're mostly staffed by nurse practitioners but there is always at least one doctor on-site as well, my family have used these from time-to-time over the years (getting GP appointments is someimes as bad here as the UK) an found them to be quite good.
Maybe an expansion of this type of facility is what the UK needs?
africanspur
Full Member
- Joined
- Sep 1, 2010
- Messages
- 10,012
- Supports
- Tottenham Hotspur
I went for an executive board-level job at the trust earlier this year (having worked exclusively in the private sector). As part of the interview process I did an engagement exercise with the directors of various specialties and operating departments. They were the most soulless uninspiring group of people I’ve ever sat with. Less energy and optimism than at a funeral. After an hour I knew that this was a group of people clinging to their salaries and pension, who lacked the passion and capability to change things for the better. It was eye-opening and there was no way I’d spend the rest of my life working around such misery
It has become a generally quite depressing place to work at the clinical level in a lot of places sadly and I imagine the same is true at a managerial level too.
Changing that is important but not entirely sure how it's done really.
africanspur
Full Member
- Joined
- Sep 1, 2010
- Messages
- 10,012
- Supports
- Tottenham Hotspur
I'm glad I started this thread, it seems quite a few posters have observations that are worthy of more discussion, for my part I'll add this:
In the US as an alternative to A&E (or the ER as they call it here) most areas have a number of what's called Urgent Care facilities, I know that the UK has some of these but just how widespread and accesible are they?
In my local area the main hospital is 3 miles away and in a 5 mile radius there's at least half a dozen of these facilities, they're open 8am to 8pm 7 days a week and are first come, first served with no appointments.
They're mostly staffed by nurse practitioners but there is always at least one doctor on-site as well, my family have used these from time-to-time over the years (getting GP appointments is someimes as bad here as the UK) an found them to be quite good.
Maybe an expansion of this type of facility is what the UK needs?
It's a good question. My view is sadly quite London centric but we certainly do have quite a few of them across London at least. Some of them were previously full on A&Es which have closed down.
Most A&Es will also have an urgent care portion within their A&E proper too to filter through some of the stuff that is neither an accident or emergency. Especially within these, they will be staffed by NPs, as well as GPs.
They do work well like you said and stop the ED physicians from having to see the person who's had a headache for 3 weeks.
Red in STL
Turnover not takeover
Is that really true though, I've no doubt it was better then than now but incredible levels seems a stretch to meI don’t think the problem with the NHS is strictly the healthcare model.
With a functioning economy, adequate funding and the will to take a detailed look at imigration, the free at the point of care healthcare we have enjoyed can return to the incredible levels of satisfaction we saw 15-20 years ago.
The true issue at play is social care. We have a rapidly aging population, living longer than ever with mounting health ailment's that are having to be absorbed into the NHS because the care system can’t cope, this is then adding an extra boot onto the neck of the NHS which is already under strain from austerity, covid and labour issues.
We need a means of funding elderly care that’s sustainable and isn’t just shunting people into A&E or overcrowded wards, or booking up every gp appointment because they want a chat about one of their 16 minor health conditions.
isn’t an easy answer to this, I’d be happy personally if there was a new tax created that acted almost as a pension so that people aren’t having to sell their homes to live in a shithole care home but that’s just me. Money has to come from somewhere.
You're not wrong about social care. and that plays in to what should and what shouldn't the NHS do, social care used to be the remit of local government, not the NHS, and IMO that needs to be either reverted back tp local goverment responsibility or a new system independent of both but state-finded
T00lsh3d
Has massive thighs.
- Joined
- Mar 20, 2014
- Messages
- 10,365
That’s an under-rated element of the problem: how do you change the culture of such big organisations? Where the defeatism and misery is so embedded. I’ve asked lots of people over the years and have never had a compelling answer. In fact the only consistent answer I’ve had is, “you can’t”It has become a generally quite depressing place to work at the clinical level in a lot of places sadly and I imagine the same is true at a managerial level too.
Changing that is important but not entirely sure how it's done really.
Red in STL
Turnover not takeover
The main problem I see with these in the UK is how do you get to them, outside of major cities in the US public transport is non-existent so everyone drives, whilst the UK is better with public transport it still doesn't reach the levels where it would be needed most and driving is less of an option as wellIt's a good question. My view is sadly quite London centric but we certainly do have quite a few of them across London at least. Some of them were previously full on A&Es which have closed down.
Most A&Es will also have an urgent care portion within their A&E proper too to filter through some of the stuff that is neither an accident or emergency. Especially within these, they will be staffed by NPs, as well as GPs.
They do work well like you said and stop the ED physicians from having to see the person who's had a headache for 3 weeks.
Paul the Wolf
Former Score Predictions Comp Organiser (now out)
Is that really true though, I've no doubt it was better then than now but incredible levels seems a stretch to me
You're not wrong about social care. and that plays in to what should and what shouldn't the NHS do, social care used to be the remit of local government, not the NHS, and IMO that needs to be either reverted back tp local goverment responsibility or a new system independent of both but state-finded
The last time I used the NHS was in the mid 2000's and I thought it was so poor then - how bad is it now?
Habs
Full Member
- Joined
- Aug 23, 2015
- Messages
- 739
So how did I not read it?
Nothing I said indicates that I didn't read the post. I'm saying that somehow, despite the BMA apparently being this boogeyman who gets amazing terms for GPs. Yet despite this, a third of GPs want to quit within 5 years. 20% of (fully qualified!!) GPs under the age of 30 quit last year.
Why people think doctors should be paid the same for working on a Sunday morning as a Tuesday afternoon I have no idea really. I certainly wouldn't expect to be paying a plumber or lawyer the same.
I've worked as a (hospital) doctor in 4 different countries and have friends and colleagues working in others which I have not. Through circumstance that I won't bother getting into, the UK is where I've ended up staying and working and honestly the way doctors are seen here in this country compared to the other countries is....baffling.
I’ve seen your posts on here over the years, and I respect the effort you’ve put in to try to educate people about what’s really happening.
I’ve stopped bothering to be honest and given up long ago. I mean why even bother responding to such ridiculous posts- if someone replies like that you know they have absolutely no idea what’s really happening to the NHS and more importantly they’ll never change their perspective and will only listen to what they want.
I always lived in the same city, never thought about leaving here, but I realised that there’s no future for doctors in the UK. Both me and my wife recently CCT’d as GP’s and are moving abroad in the next 6 months. We’ve been offered triple our UK salaries for a 40 hour week. When we were interviewing for these posts it felt like we were on another planet.
Floodgates have opened, and the amount of doctors leaving the UK is crazy. Almost everyone I have spoken to or worked with under <35 had the same plan, because it’s a no brainer.
It’s a really sad time for the British population and I worry for my parents. People think they’re suffering now, but the next 10-15 years are going to be really painful
Oo0AahCantona
Full Member
- Joined
- May 23, 2014
- Messages
- 5,490
Is that really true though, I've no doubt it was better then than now but incredible levels seems a stretch to me
You're not wrong about social care. and that plays in to what should and what shouldn't the NHS do, social care used to be the remit of local government, not the NHS, and IMO that needs to be either reverted back tp local goverment responsibility or a new system independent of both but state-finded
I mean, it’s a difficult question to answer, all we can look at is anecdotal evidence and the satisfaction data and the world health index.
mid 2000’s satisfaction was at an all time
High, like most of life it’s a postcode lottery, I’ve never had anything but amazing care in Cambridgeshire, and while people have banged on about gp appointments for years it’s only something I’ve had to notice in the past 4/5 years.
reality is we have had a healthcare system that by and large worked, was well above average in metrics and was free at the point of use. It isn’t that system anymore.
im not married to the nhs being completely free, but moving to an American style model is a hill I’m literally willing to die on and would genuinely look to physically fight back against, I feel that strongly against it. The principles of the NHS are immensely valuable.
Red in STL
Turnover not takeover
I can't speak to personal experience as 2011 was the last time I used it but it wasn't that great then.The last time I used the NHS was in the mid 2000's and I thought it was so poor then - how bad is it now?
However my parents and siblings still use the system, my mother was taken ill 18 months or so ago and had to be taken by ambulance to hospital, the ambulance took more than 2 hours to arrive and then she had to wait in the ambulance for about 7 hours at the hospital because there wasn't a bed available, eventually she was admitted and spent a week there, this was at Royal Cornwall Hospital in Truro, the main hospital in Cornwall.
One of my brothers was recently told he needs aortic valve surgery, this is the second most common cardiac procedure and there isn't a hospital in Cornwall that does this surgery so he'll have to go to Plymouth in Devon, to me it's a scandal of epic proportions that the second most common cardiac procedure can't be done in a county with a population of over half a million
Eplel
Full Member
- Joined
- May 15, 2016
- Messages
- 2,404
The problem is that successive governments see the NHS as a cost.
It's not a cost, it's an investment - a healthier and more productive population is the reward to reap.
It's not a cost, it's an investment - a healthier and more productive population is the reward to reap.
Red in STL
Turnover not takeover
As someone who now lives in the US you won't get an argument from me on that!I mean, it’s a difficult question to answer, all we can look at is anecdotal evidence and the satisfaction data and the world health index.
mid 2000’s satisfaction was at an all time
High, like most of life it’s a postcode lottery, I’ve never had anything but amazing care in Cambridgeshire, and while people have banged on about gp appointments for years it’s only something I’ve had to notice in the past 4/5 years.
reality is we have had a healthcare system that by and large worked, was well above average in metrics and was free at the point of use. It isn’t that system anymore.
im not married to the nhs being completely free, but moving to an American style model is a hill I’m literally willing to die on and would genuinely look to physically fight back against, I feel that strongly against it. The principles of the NHS are immensely valuable.
The NHS isn't completely free now anyway, dental treatment has always had a cost associated with it and then there's prescriptions and vision
I never thought I'd ever say this, but therer are areas that perhaps should be run by private companies though funded by the taxpayer, the reality is that the NHS is highly inefficient in some areas and it would likely be cheaper to outsource some services because private companies will not tolerate those kind of inefficences, as long as the service is better and cheaper then it might be the way too go.
Red in STL
Turnover not takeover
Nope, governments of the party that just got booted out see the NHS as way to make moneyThe problem is that successive governments see the NHS as a cost.
It's not a cost, it's an investment - a healthier and more productive population is the reward to reap.
maximus419
Full Member
I don't know what the options are for the NHS but I do have a friend who has personally had experience of it and to say it's not fit for purpose is an understatement.
His mum had pains in her stomach and was on two occasions basically fobbed off by her GP. He had recently spent 3 months sectioned after a psychotic episode and has been terribly treated and during his stay in hospital his mum was taken into hospital after being in terrible pain again. She's now been told after waiting over 3 weeks for a telephone call which didn't happen initially and had to wait another week that she had cancer and it's got into her bowel and is basically inoperable.
Worst of all there has been zero follow up by her GP. No treatment options, literally just left to fend for themselves. My friend since came out off his section but is in no way in a position to now care for his dying mum. Clearly this will worsen his own mental state and I suspect there is a strong possibility he goes completely off the rails trying to deal with all this.
It's an absolute scandal the state the NHS has been allowed to get into. And whilst I blame the previous govt, I also feel standards within the NHS have fallen far below what they should be. The staff also need a huge change in approach and professionalism, the mistakes, the lack of care for patients, it's rotten throughout.
How do you fix this given the state it's in? Worse of all, I suspect over the coming months we are going to hear some awful stories and potential legal action taken against the NHS for neglect. I think they will be destroyed by the legal payouts and wouldn't be surprised if it collapses completely as the govt will run out of money to keep it going.
His mum had pains in her stomach and was on two occasions basically fobbed off by her GP. He had recently spent 3 months sectioned after a psychotic episode and has been terribly treated and during his stay in hospital his mum was taken into hospital after being in terrible pain again. She's now been told after waiting over 3 weeks for a telephone call which didn't happen initially and had to wait another week that she had cancer and it's got into her bowel and is basically inoperable.
Worst of all there has been zero follow up by her GP. No treatment options, literally just left to fend for themselves. My friend since came out off his section but is in no way in a position to now care for his dying mum. Clearly this will worsen his own mental state and I suspect there is a strong possibility he goes completely off the rails trying to deal with all this.
It's an absolute scandal the state the NHS has been allowed to get into. And whilst I blame the previous govt, I also feel standards within the NHS have fallen far below what they should be. The staff also need a huge change in approach and professionalism, the mistakes, the lack of care for patients, it's rotten throughout.
How do you fix this given the state it's in? Worse of all, I suspect over the coming months we are going to hear some awful stories and potential legal action taken against the NHS for neglect. I think they will be destroyed by the legal payouts and wouldn't be surprised if it collapses completely as the govt will run out of money to keep it going.
Health care is non negotiable. Just work out how much it will cost for good heathcare then get the money through taxes. It's that simple.
How much tax do you think the government can squeeze out of the tax payer?
africanspur
Full Member
- Joined
- Sep 1, 2010
- Messages
- 10,012
- Supports
- Tottenham Hotspur
The BMA smashing it here.
Abizzz
Full Member
- Joined
- Mar 28, 2014
- Messages
- 8,673
Wasn't that basically the tory approach? The new government might want to try something else.I think they should get rid of health care completely and let everybody die.
africanspur
Full Member
- Joined
- Sep 1, 2010
- Messages
- 10,012
- Supports
- Tottenham Hotspur
There definitely isn't an easy fix for the NHS. Frankly, healthcare as a whole across the world will probably need a significant rethink as our populations become older and more multi-morbid, people live longer and treatments become better at keeping people alive (and more expensive).
In terms of spit balling ideas though:
-The easiest one is more resources of course. Yes its a 'money sink'. But it is indisputable that the UK is below the average for doctors, nurses and beds per 100,000 population for OECD countries. That leads to a system that is constantly stretched, constantly just about surviving, constantly making do rather than actually trying to provide high quality care. That means for funding, updating infrastructure, paying staff appropriately so you actually attract and retain good, happy people.
-Improvements in social care. A significant part of the pressure comes from not being able to discharge some patients, some for a long time, because of failures in the social care system. At best, its waiting for equipment to be delivered or for for a care package to be implemented. At worst, its waiting because someone's family has decided to go on holiday and don't want to come back early to take their relative back or a homeless person. Hospitals should be primarily for sorting out acute medical issues, not social issues. This should also include an increase in pay and standing of care workers.
-I think outlining how much things cost to patients when they're sent for an appointment or scans may be helpful to reduce non-attendance (which is ridiculous).
-Increased focus on preventative care (particularly with obesity and alcohol) and improved health literacy of the population. The social determinants of health and the inequities we see across the country are shocking.
-Incentives for innovation and changes. I'll be honest and say I don't really know how to do this. Currently, you could be an amazing consultant, average or shocking (or nurse) and you will get paid essentially the same. Beyond pride, there is little incentive to poke your head above the parapet and do things differently and that needs to change. In some areas of the country, entire regions are joining together. Which is good for some things but means changes often have to happen on a regional level, which can be glacial.
-I'll go slightly against the grain and say we actually probably need more managers, not less. But with the proviso that we encourage more clinical managers too. We actually have less managers than, again, most of our OECD peers.
-I'm nowhere near as against the idea of European/ Australasian style private insurance existing alongside the public health system.
In terms of spit balling ideas though:
-The easiest one is more resources of course. Yes its a 'money sink'. But it is indisputable that the UK is below the average for doctors, nurses and beds per 100,000 population for OECD countries. That leads to a system that is constantly stretched, constantly just about surviving, constantly making do rather than actually trying to provide high quality care. That means for funding, updating infrastructure, paying staff appropriately so you actually attract and retain good, happy people.
-Improvements in social care. A significant part of the pressure comes from not being able to discharge some patients, some for a long time, because of failures in the social care system. At best, its waiting for equipment to be delivered or for for a care package to be implemented. At worst, its waiting because someone's family has decided to go on holiday and don't want to come back early to take their relative back or a homeless person. Hospitals should be primarily for sorting out acute medical issues, not social issues. This should also include an increase in pay and standing of care workers.
-I think outlining how much things cost to patients when they're sent for an appointment or scans may be helpful to reduce non-attendance (which is ridiculous).
-Increased focus on preventative care (particularly with obesity and alcohol) and improved health literacy of the population. The social determinants of health and the inequities we see across the country are shocking.
-Incentives for innovation and changes. I'll be honest and say I don't really know how to do this. Currently, you could be an amazing consultant, average or shocking (or nurse) and you will get paid essentially the same. Beyond pride, there is little incentive to poke your head above the parapet and do things differently and that needs to change. In some areas of the country, entire regions are joining together. Which is good for some things but means changes often have to happen on a regional level, which can be glacial.
-I'll go slightly against the grain and say we actually probably need more managers, not less. But with the proviso that we encourage more clinical managers too. We actually have less managers than, again, most of our OECD peers.
-I'm nowhere near as against the idea of European/ Australasian style private insurance existing alongside the public health system.
africanspur
Full Member
- Joined
- Sep 1, 2010
- Messages
- 10,012
- Supports
- Tottenham Hotspur
That’s an under-rated element of the problem: how do you change the culture of such big organisations? Where the defeatism and misery is so embedded. I’ve asked lots of people over the years and have never had a compelling answer. In fact the only consistent answer I’ve had is, “you can’t”
Yep, very true. Just a recent depressing example of how the NHS often treats its employees.
One of our nurse managers (who is very good) has had their own office for years. They need it really, as their work involves quite a bit of people management and sensitive discussions, meetings etc. She's quite senior and maybe 5 years away from retirement. There's been some renovations in the department recently.
Someone came to her, while she was in the office, and told her she had 20 minutes to vacate her office as it was being given to someone else, and she would be hot desking instead. This isn't a one off and I've heard similar stories from colleagues.
The service is also sadly awash with stories of non consultant doctors having to beg and fight to get annual leave for their own wedding, when placed on various on call shifts during it, as well as many others.
Its really not a good employer.
T00lsh3d
Has massive thighs.
- Joined
- Mar 20, 2014
- Messages
- 10,365
Do you think the NHS will keep its elective care in-house going forward? Or can you see it being outsourced and the NHS’s focus being on ED, cancer, non-surgical etc etcThere definitely isn't an easy fix for the NHS. Frankly, healthcare as a whole across the world will probably need a significant rethink as our populations become older and more multi-morbid, people live longer and treatments become better at keeping people alive (and more expensive).
In terms of spit balling ideas though:
-The easiest one is more resources of course. Yes its a 'money sink'. But it is indisputable that the UK is below the average for doctors, nurses and beds per 100,000 population for OECD countries. That leads to a system that is constantly stretched, constantly just about surviving, constantly making do rather than actually trying to provide high quality care. That means for funding, updating infrastructure, paying staff appropriately so you actually attract and retain good, happy people.
-Improvements in social care. A significant part of the pressure comes from not being able to discharge some patients, some for a long time, because of failures in the social care system. At best, its waiting for equipment to be delivered or for for a care package to be implemented. At worst, its waiting because someone's family has decided to go on holiday and don't want to come back early to take their relative back or a homeless person. Hospitals should be primarily for sorting out acute medical issues, not social issues. This should also include an increase in pay and standing of care workers.
-I think outlining how much things cost to patients when they're sent for an appointment or scans may be helpful to reduce non-attendance (which is ridiculous).
-Increased focus on preventative care (particularly with obesity and alcohol) and improved health literacy of the population. The social determinants of health and the inequities we see across the country are shocking.
-Incentives for innovation and changes. I'll be honest and say I don't really know how to do this. Currently, you could be an amazing consultant, average or shocking (or nurse) and you will get paid essentially the same. Beyond pride, there is little incentive to poke your head above the parapet and do things differently and that needs to change. In some areas of the country, entire regions are joining together. Which is good for some things but means changes often have to happen on a regional level, which can be glacial.
-I'll go slightly against the grain and say we actually probably need more managers, not less. But with the proviso that we encourage more clinical managers too. We actually have less managers than, again, most of our OECD peers.
-I'm nowhere near as against the idea of European/ Australasian style private insurance existing alongside the public health system.
africanspur
Full Member
- Joined
- Sep 1, 2010
- Messages
- 10,012
- Supports
- Tottenham Hotspur
Do you think the NHS will keep its elective care in-house going forward? Or can you see it being outsourced and the NHS’s focus being on ED, cancer, non-surgical etc etc
I think it should and will.
A health service does have to think about health economics to at least some extent, especially one that aims to be a universal health service like the NHS.
Giving up all the 'easy' elective money making care (orthopaedic procedures, opthalmology, endoscopy etc) would be a mistake I think.
Mainoonited
Full Member
- Joined
- Nov 27, 2023
- Messages
- 619
Many people from my family and friends circle work in the NHS, from my conversations with them the below are a few of the big issues the NHS faces.
1. Bed blockers. Old people blocking beds in wards because they are not healthy enough to go home and look after themselves and they don't have anyone to care for them. Back in the day there used to be seperate care facilities people like this could be shifted too.
2. Under paid permanent staff, expensive contractors. This BS cycle needs to end. NHS staff are underpaid, they quit, contractors are bought in to replace them (some even get paid less), but the companies who provide the resource charge a boatload. Some nurses quit and join agencies just to get a pay rise and better conditions. Some agencies use foreign staff and pay them even less, but still charge way more than it would cost to give permament staff a pay rise.
3. Outsourcing everything. Laundry, cleaning, kitchens, you name it, it's outsourced. The more people involved, the more money spent.
4. Too much management and poor IT systems.
It sounds wierd, but to ultimately spend less money, you need to initially spend more money - or at least spend money in the right places.
1. Bed blockers. Old people blocking beds in wards because they are not healthy enough to go home and look after themselves and they don't have anyone to care for them. Back in the day there used to be seperate care facilities people like this could be shifted too.
2. Under paid permanent staff, expensive contractors. This BS cycle needs to end. NHS staff are underpaid, they quit, contractors are bought in to replace them (some even get paid less), but the companies who provide the resource charge a boatload. Some nurses quit and join agencies just to get a pay rise and better conditions. Some agencies use foreign staff and pay them even less, but still charge way more than it would cost to give permament staff a pay rise.
3. Outsourcing everything. Laundry, cleaning, kitchens, you name it, it's outsourced. The more people involved, the more money spent.
4. Too much management and poor IT systems.
It sounds wierd, but to ultimately spend less money, you need to initially spend more money - or at least spend money in the right places.
T00lsh3d
Has massive thighs.
- Joined
- Mar 20, 2014
- Messages
- 10,365
Logical and I agree. It just doesn’t seem to go along with what’s actually happening on the ground. I can only really speak for my experience with trusts in the north, but elective care doesn’t seem to be getting better and the reality is; if you replace Doris’s hip at 2 weeks she’s in and out in 2 days…..if you replace at 104 weeks now that she’s had 2 years to get fat and immobile, she’s clogging the bed for a week. And you already didn’t have any spare bedsI think it should and will.
A health service does have to think about health economics to at least some extent, especially one that aims to be a universal health service like the NHS.
Giving up all the 'easy' elective money making care (orthopaedic procedures, opthalmology, endoscopy etc) would be a mistake I think.
What’s your experience in the south like recently?
Munkehboi
Full Member
Agree with the issues with social care. As a B6 nurse on an acute/general medical ward I can tell you the majority of patients are awaiting placements or a care package. Since COVID we've seen such a huge rise in social admissions and mental health. Care homes are not coping with patients with multiple co-morbidities. There's been a huge spike of delirium patients, most with dementia who keep falling so they send them into hospital and refuse to have them back until they are at their baseline. Rarely are they ever back to their baseline the though. We are seeing an incredible amount of elderly patients who have been independent, living at home and now needing placements and its just clogging up the whole system.I don’t think the problem with the NHS is strictly the healthcare model.
With a functioning economy, adequate funding and the will to take a detailed look at imigration, the free at the point of care healthcare we have enjoyed can return to the incredible levels of satisfaction we saw 15-20 years ago.
The true issue at play is social care. We have a rapidly aging population, living longer than ever with mounting health ailment's that are having to be absorbed into the NHS because the care system can’t cope, this is then adding an extra boot onto the neck of the NHS which is already under strain from austerity, covid and labour issues.
We need a means of funding elderly care that’s sustainable and isn’t just shunting people into A&E or overcrowded wards, or booking up every gp appointment because they want a chat about one of their 16 minor health conditions.
isn’t an easy answer to this, I’d be happy personally if there was a new
Sadly, the mental health patients don't belong on an acute medical ward and their MH needs are just burning out the work force. My ward currently has two patients with violence and ligature risk assessments - this was rarely a thing when I first qualified. Now we are seeing more and more suicide attempts and aggression towards staff. So many of my peers are off work, injured or through stress. Since the NMC members agreed a 5% pay rise last year, NHSp (pool/bank staff) have conveniently cut their hourly pay quite substantially so we are seeing more and more unfilled staffing gaps. We're seeing newly qualified nurses choosing community and clinics instead of acute hospital care nowadays as well. They understand how difficult it is and I can't blame them for taking a less stressful role.
People are getting older, living longer but there aren't more beds in the hospitals. In fact my trust has less beds since I started working here however, since 2000, the population in my area has increased by approx 98,000. The pressures of patient flow keeps mounting to move ambulances on to their next patients and keep the ED corridors clear but there are more re-admissions than ever before because we are unsafely discharging patients home. More funding needs to be in place for social care and MH and that funding needs to be spent wisely and effectively. Being in the NHS for so long, I won't hold my breath for anything close to this happening though.
On a side note our international nurses find the cultural differences quite strange and sometimes distressing. They always ask why the families are not looking after the elderly? I think the socio/cultural differences in how we look after our elderly loved ones impact the NHS more than we think about sometimes.
Red in STL
Turnover not takeover
This is nuts .... and I guess shows the scale of the problem
One of my brothers, who works as contractor for the NHS, needs an aortic valve replacement, a major but fairly common surgery, he lives in Camborne, Cornwall.
This surgery cannot be done in Cornwall, apparently the NHS doesn't have the capability in the county, despite having a major hospital 13 mles away he had to to go to Plymouth in Devon 66 mles away.
Now he's been informed that the surgery will take place later this month, at a private hospital in London 300 miles away, the NHS pays for it all including the transportation to and from Cornwall, the extra cost must be staggering!
One of my brothers, who works as contractor for the NHS, needs an aortic valve replacement, a major but fairly common surgery, he lives in Camborne, Cornwall.
This surgery cannot be done in Cornwall, apparently the NHS doesn't have the capability in the county, despite having a major hospital 13 mles away he had to to go to Plymouth in Devon 66 mles away.
Now he's been informed that the surgery will take place later this month, at a private hospital in London 300 miles away, the NHS pays for it all including the transportation to and from Cornwall, the extra cost must be staggering!
Ronaldo's Love Child
Full Member
- Joined
- Aug 2, 2018
- Messages
- 656
The last time I used the NHS was in the mid 2000's and I thought it was so poor then - how bad is it now?
8-12 hour waits in A & E and could be longer.
Ronaldo's Love Child
Full Member
- Joined
- Aug 2, 2018
- Messages
- 656
Agree with the issues with social care. As a B6 nurse on an acute/general medical ward I can tell you the majority of patients are awaiting placements or a care package. Since COVID we've seen such a huge rise in social admissions and mental health. Care homes are not coping with patients with multiple co-morbidities. There's been a huge spike of delirium patients, most with dementia who keep falling so they send them into hospital and refuse to have them back until they are at their baseline. Rarely are they ever back to their baseline the though. We are seeing an incredible amount of elderly patients who have been independent, living at home and now needing placements and its just clogging up the whole system.
Sadly, the mental health patients don't belong on an acute medical ward and their MH needs are just burning out the work force. My ward currently has two patients with violence and ligature risk assessments - this was rarely a thing when I first qualified. Now we are seeing more and more suicide attempts and aggression towards staff. So many of my peers are off work, injured or through stress. Since the NMC members agreed a 5% pay rise last year, NHSp (pool/bank staff) have conveniently cut their hourly pay quite substantially so we are seeing more and more unfilled staffing gaps. We're seeing newly qualified nurses choosing community and clinics instead of acute hospital care nowadays as well. They understand how difficult it is and I can't blame them for taking a less stressful role.
People are getting older, living longer but there aren't more beds in the hospitals. In fact my trust has less beds since I started working here however, since 2000, the population in my area has increased by approx 98,000. The pressures of patient flow keeps mounting to move ambulances on to their next patients and keep the ED corridors clear but there are more re-admissions than ever before because we are unsafely discharging patients home. More funding needs to be in place for social care and MH and that funding needs to be spent wisely and effectively. Being in the NHS for so long, I won't hold my breath for anything close to this happening though.
On a side note our international nurses find the cultural differences quite strange and sometimes distressing. They always ask why the families are not looking after the elderly? I think the socio/cultural differences in how we look after our elderly loved ones impact the NHS more than we think about sometimes.
This resonates with me deeply.
My mother is 96 and has Alzheimers.
She's lived in her own home for 63 years. Only the last year it has become challenging, not helped by her failing eyesight (AMD).
I've employed private live in carers after she had a recent fall and broke her clavicle. She developed delirium (shocking if you've never seen it before). There was no rush to discharge her. She wasn't eating well and I realised that if she stays much longer then she will deteriorate, hence the private live in carers.
Having carers with her all the time helped. We got my mum to have one more Christmas in her house but unfortunately in Feb she fell, paramedics detected AF and she ended up in hospital (also with pneumonia).
From that moment on I lost control of her care.
During initial hospital admission she was on a trolley bed with many others lined up in a row. Often she needed the toilet but staff were too busy to attend and so the inevitable would occur.
They eventually found her a bed and long story-short.....she stayed in hospital for 5 weeks, being constantly moved from ward to ward.
The care she received was akin to the care a mechanic has when trying to fix a car. There is SOME care there but once a certain part is fixed then the car is just parked waiting for collection.
The staff didn't have time to help her to eat properly. She became very very weak. When I asked if they were giving her any physical therapy I received vague replies that yes, when he physio team visit......but no indication as to how often they visited her. Upon closer scrutiny, I realised she was getting no therapy as when she was asked if she wanted to participate she would say "no"......probably because she was half asleep.
I asked the staff if they could help her out of bed and sit in the bedside chair but they told me they couldn't lift her in case they hurt themselves so would have to wait for the physio team to do it and of course, no idea if that message was ever relayed to the physio team or not.
Other days she'd be sat in the armchair so presumably some nurses were happy to assist her whilst other were not.
Mum wasn't incontinent when she arrived in hospital but she soon became so. Elderly patients (possibly the dementia ones) were fitted with pads. I witnessed one lady in my mum's ward scream for assistance in needing the toilet. No-one came and shortly after she screamed "I'm sorry. I'm sorry" as she must have relieved herself in bed.
Mum started to waste away in hospital. Having no choice but to lie in bed all day, every day for 5 weeks led to her becoming end of life. She was finally discharged to a care home and thankfully recovered physically to some degree thanks to the care staff having more time to encourage her to eat and drink but unfortunately, mentally, mum has declined badly now.
The mechanic analogy I used earlier is accurate I think. The hospital treated her succesfully for the pneumonia and the AF but that was it. As a direct result of her stay in hospital my mum can no longer walk or stand up (she was walking the day before her hospital admission).
No holistic treatment or thoughts as to how do we get this lady back to her baseline.
So the conlusion? The NHS can be bloody brilliant at times but if often appalling
BlueMoonOutcast
Rag in Disguise
The NHS may as well not exist for me. I'm neurodivergent and have a sensitivity to sound. This means I wear earbuds a lot and it causes me to have ear issues from time to time.
One of my ears was blocked and I was partially deaf and it was causing pressure in my head. NHS24 refused to have me seen and my gp wouldn't give me an appointment. Just straight up "we have no appointments sorry".
I called into a private clinic a half hours drive from me and was seen that morning. All sorted and cleared with a little after care for under £50.
I wish I could cancel my national insurance.
One of my ears was blocked and I was partially deaf and it was causing pressure in my head. NHS24 refused to have me seen and my gp wouldn't give me an appointment. Just straight up "we have no appointments sorry".
I called into a private clinic a half hours drive from me and was seen that morning. All sorted and cleared with a little after care for under £50.
I wish I could cancel my national insurance.
Alex99
Rehab's Pete Doherty
- Joined
- May 30, 2009
- Messages
- 17,909
This is nuts .... and I guess shows the scale of the problem
One of my brothers, who works as contractor for the NHS, needs an aortic valve replacement, a major but fairly common surgery, he lives in Camborne, Cornwall.
This surgery cannot be done in Cornwall, apparently the NHS doesn't have the capability in the county, despite having a major hospital 13 mles away he had to to go to Plymouth in Devon 66 mles away.
Now he's been informed that the surgery will take place later this month, at a private hospital in London 300 miles away, the NHS pays for it all including the transportation to and from Cornwall, the extra cost must be staggering!
We're going back over 15 years, but my grandfather had to travel from the heart of Snowdonia to a hospital in London for some cancer treatment, because apparently nowhere else in the country could do it.
thisisnottaken1
Full Member
It’s disgraceful. It’s been underfunded for at least 15 years now. It needs to be fully renationalised and properly funded. But Slimy Streeting wants it gone completely
Fully Fledged
Would risk it all for the Colonel
https://change.nhs.uk/en-GB/projects/start-here
Have your say. Fill in the survey to give your opinion on The NHS, and what needs to be done to improve it.
Have your say. Fill in the survey to give your opinion on The NHS, and what needs to be done to improve it.
So, Wes Streeting is bringing in “football style” league tables for NHS trusts. God help those that come bottom.
Not sure how I feel about this
Not sure how I feel about this
Share:
